Table of Contents
One effective way to curb the opioid epidemic is through the use of medications like Suboxone as part of a medication-assisted treatment (MAT) program. But if you ever feel the need or want to get off of Suboxone what does Suboxone Withdrawal look like?
More than 2.1 million people in the U.S. (16 million globally) have an opioid use disorder? And even more concerning, opioids (especially synthetics like fentanyl and stimulants such as cocaine or methamphetamine) account for 75% of drug overdose deaths—with the rates increasing in recent years.
Suboxone has proven to be an effective tool in helping reduce cravings and withdrawal symptoms experienced by people with opioid use disorder. It provides a much-needed lifeline to those fighting the battle against opioid addiction.
But due to how it works (i.e., by occupying opioid receptors), individuals can experience Suboxone withdrawal symptoms when the medication is stopped. Understanding the symptoms of Suboxone withdrawal is crucial so that one can prepare themselves for the road ahead and seek professional help if needed.
What is Suboxone—and How Does it Work?
People with opioid use disorder constantly battle with an overpowering desire to use the substances, may develop an increased tolerance to the opioids, and have to deal with debilitating withdrawal symptoms when opioid use is discontinued.
For those seeking a new life, breaking free from the chains of opioid addiction can be an incredibly difficult and painful experience. But medications like Subutex and Suboxone can make the recovery journey easier and more manageable.
Suboxone is a medication approved by the FDA for treating opioid use disorder. It’s available in different strengths and is administered sublingually (under the tongue) or buccally between your gums and cheek.
The brand name Suboxone refers to a combination of two active ingredients: buprenorphine and naloxone. Each ingredient serves a different purpose—but they work together to reduce opioid misuse by helping manage cravings and withdrawal symptoms.
Buprenorphine’s Role
Buprenorphine is a partial opioid agonist, which means it only partially activates opiate receptors. Its partial agonism is a unique quality that allows its analgesic effects to plateau at higher doses before it becomes antagonistic.
And unlike full-opioid agonists like fentanyl and morphine, buprenorphine is less likely to cause a high (euphoria)—thus reducing harms associated with opioid misuse and allowing for milder withdrawal symptoms.
But while Suboxone is an effective drug on the road to recovery from opiate dependence, it can also be addictive. As a partial opioid agonist (buprenorphine), you may experience Suboxone withdrawal symptoms.
Naloxone’s Role
On the other hand, naloxone is an opioid antagonist that works by blocking or reversing the effects of harmful opioid drugs. It works by blocking the brain’s uptake of opioids.
Naloxone competes for space on opiate receptors with opioids—but due to its high affinity for the receptors, it can ‘boot’ or ‘take up the space’ before heroin, fentanyl, oxycodone, and other harmful opioids come along.
Please Note: While Suboxone is useful for helping patients overcome addiction, it’s not a magic pill. The medication should be viewed as nothing more than a key component of a comprehensive opioid addiction treatment plan that includes counselling and behavioral therapy.
Suboxone Withdrawal Symptoms
If you’re prescribed Suboxone for the treatment of opioid use disorder (or any other off-label use), you are at risk of physical and psychological dependence. You may experience uncomfortable withdrawal symptoms if you attempt to stop abruptly or miss a dose.
The drug-seeking and drug-craving behavior can also lead to misuse or abuse. Those affected may take the opioid medication in a way that’s not prescribed, exposing them to dangerous side effects—especially when combined with other drugs.
The severity of symptoms and the Suboxone withdrawal timeline can vary depending on several factors—including the dosage taken and the length of time the medication was used. Here are some common physical and psychological symptoms of Suboxone withdrawal:
Physical Suboxone Withdrawal Symptoms
The physical symptoms of Suboxone withdrawal are similar to typical opioid withdrawal symptoms but are usually not as severe as those experienced with harsh drugs like fentanyl. Regardless, they can be challenging to manage. The physical symptoms can include:
- Nausea and vomiting
- Diarrhea
- Tremors
- Muscle aches and pains
- Headaches
- Sweating
- Fatigue
- Insomnia
- Cold-like symptoms
Psychological/Emotional Symptoms of Suboxone Withdrawal
On top of the uncomfortable physical symptoms, people may also experience the following psychological challenges associated with Suboxone withdrawal.
- Anxiety
- Agitation
- Difficulty concentrating
- Restlessness
- Depression
- Irritability
- Cravings for Suboxone or other opioids
- Mood swings
Please keep in mind that some of the psychological Suboxone withdrawal symptoms may be a “resurfacing” of mental health issues suppressed by drug use. Individuals may also struggle with an exhausting and overwhelming feeling of guilt and regret when they see the damage caused by their addiction problem.
Regardless, it’s crucial to seek help to manage the symptoms and reduce the risk of relapse. Healthcare professionals or support groups can help you to manage Suboxone withdrawal symptoms and stay on track with your recovery.
Suboxone Withdrawal Timeline
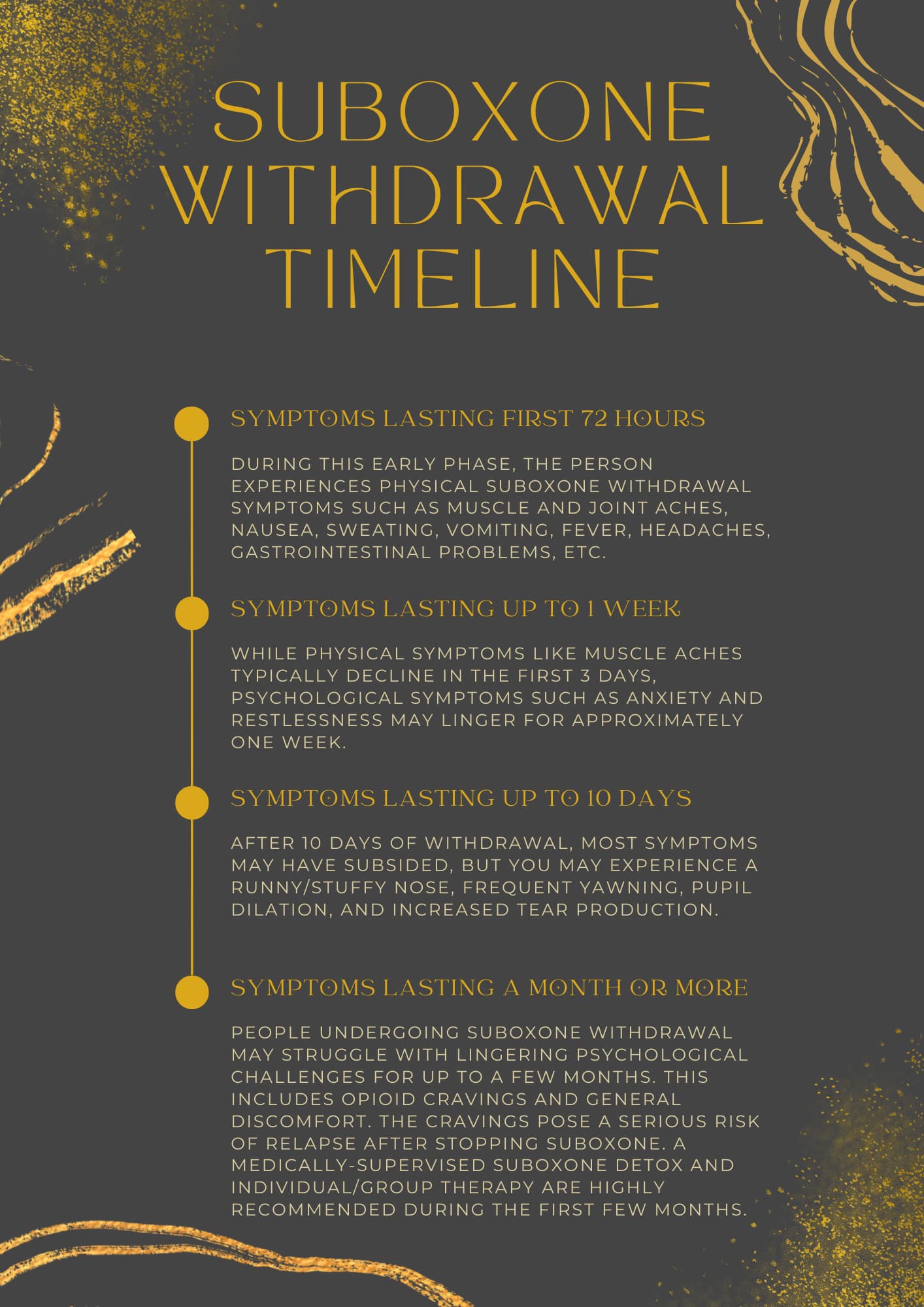
How long does Suboxone withdrawal last? One of the qualities that make Suboxone an effective treatment for opioid addiction and dependence is its long-acting effects. Suboxone withdrawal symptoms are not only milder than other opioids, but they also don’t set in as quickly. This can be attributed to buprenorphine’s relatively long half-life of 38 hours (25 to 70 hours) after sublingual administration.
Its long-acting qualities mean that the Suboxone withdrawal timeline is somewhat longer than many other opioids—as the symptoms are delayed and extended. And while there are other factors to consider in answering the question “How long does Suboxone withdrawal last?” here’s the general Suboxone withdrawal timeline:
- Symptoms Lasting First 72 Hours: During this early phase, the person experiences physical Suboxone withdrawal symptoms such as muscle and joint aches, nausea, sweating, vomiting, fever, headaches, gastrointestinal problems, etc.
- Symptoms Lasting up to 1 Week: While physical symptoms like muscle aches typically decline in the first 3 days, psychological symptoms such as anxiety and restlessness may linger for approximately one week.
- Symptoms Lasting up to 10 Days: After 10 days of withdrawal, most symptoms may have subsided, but you may experience a runny/stuffy nose, frequent yawning, pupil dilation, and increased tear production.
- Symptoms Lasting a Month or More: People undergoing Suboxone withdrawal may struggle with lingering psychological challenges for up to a few months. This includes opioid cravings and general discomfort. The cravings pose a serious risk of relapse after stopping Suboxone. A medically-supervised Suboxone detox and individual/group therapy are highly recommended during the first few months.
While this Suboxone withdrawal timeline is a good indicator of what to expect, it’s not set in stone. The severity and duration of Suboxone withdrawal symptoms vary from person to person based on several factors. This includes the presence of co-occurring disorders, medical conditions, history of alcohol and drug use, the dosage of Suboxone taken, and the duration of use.
How to Manage Suboxone Withdrawal Symptoms
Now that we’ve outlined the common Suboxone withdrawal symptoms and answered the question “How long does Suboxone withdrawal last?” what’s next? How do we manage the symptoms to ease the withdrawal process?
When it comes to managing Suboxone withdrawal, it is important to have a clear and individualized plan in place. The goal is to ease the person’s suffering and prevent relapse for long-lasting recovery. This starts with a decision to seek help.
Tapering Down Suboxone
One important resource for those experiencing withdrawal from Suboxone is a medical detox or a tapering down program.
When you develop Suboxone dependence after using the medication for a long period, your body becomes accustomed to it. Quitting abruptly (cold turkey) can lead to severe withdrawal symptoms and a higher risk of relapse, which is not what we’re looking for.
The recommended method of quitting Suboxone treatment is undergoing a tapering down of doses under the supervision of a healthcare professional. The medical detox program may also include monitoring health markers, access to psychiatric support, medications to soothe the Suboxone withdrawal symptoms, and therapy sessions. This ensures a safe and effective withdrawal process as the body gradually adjusts to functioning without the medication.
Coping Strategies for Suboxone Withdrawal
Tapering down Suboxone is only one part of the recovery journey. The individual also needs to develop coping skills to manage cravings and triggers. This includes identifying healthy ways to manage psychological symptoms like anxiety and building a strong support system.
Here are some day-to-day habits and strategies that can help you to manage the physical and emotional symptoms of Suboxone withdrawal:
- Mindfulness and meditation to help you stay present and focused.
- Exercising regularly to release endorphins and elevate your mood.
- Healthy eating to provide your body with the nutrients it needs to heal.
- Journaling to express your feelings and emotions.
- Staying hydrated to help manage symptoms like vomiting and diarrhea.
- Acknowledging and focusing on the good in your life. You can use a gratitude jar to harness positive emotions/feelings.
- Engaging in new hobbies or social activities to distract you from the symptoms.
- Identifying a support system, such as a friend, family member, or someone who can help you through the process.
- Getting enough rest.
Remember, everyone’s journey to recovery is different. What works for one person may not work for another.
And in case you relapse, hold your head high and don’t take it as a sign of failure. Stay committed to your recovery even if you experience setbacks along the way. Develop a plan for relapse prevention, such as learning to be kind and patient with yourself as you navigate this challenging time.
FAQs
Quitting Suboxone abruptly can be dangerous and is not recommended. Doing so can lead to severe withdrawal symptoms and a higher risk of relapse. Instead, work with a healthcare professional to develop a tapering plan.
Several strategies can help manage Suboxone withdrawal symptoms. This may include seeking support from your trusted social network, practicing self-care, proper nutrition, staying positive, and developing a personalized plan under the guidance of a healthcare professional.
Yes, you can overcome the symptoms of Suboxone withdrawal by adopting the right mindset, leaning on a support network, and seeking medical guidance. It may be challenging, but long-term recovery is possible when you stay committed to your goals and seek help when needed.
The duration of Suboxone withdrawal can vary from person to person, depending on individual factors like dosage, duration of use, and overall health. However, the Suboxone withdrawal timeline can last anywhere from a few weeks to months.
Due to the cravings, uncomfortable physical symptoms, and the risk of mental health challenges, it is not recommended to withdraw from Suboxone on your own. Professional help is crucial for managing Suboxone withdrawal symptoms and ensuring a safe recovery.
While Suboxone withdrawal itself is not typically fatal, withdrawal from opioids can lead to complications like dehydration and electrolyte imbalances that can be life-threatening. Again, seeking professional help is crucial for managing these symptoms and ensuring a safe recovery.
Relapse is always a risk for individuals recovering from addiction or drug dependence. However, the risk of relapse can be effectively reduced by seeking professional help and adopting the right coping strategies.