Opioid abuse/addiction is a national crisis in the United States. According to the Centers for Disease Control and Prevention (CDC), opioids accounted for 70% of drug overdose deaths in 2018. Additionally, the U.S. loses over $78.5 billion every year in its fight against opioid abuse and addiction—including synthetic opioids, heroin, and prescription pain relievers.
One of the most effective ways to combat opioid dependence is medication-assisted treatment (MAT). It has been proven to be an effective and relatively safe way to help people recover by reducing dependence on the drugs and helping with withdrawal symptoms—hence facilitating a life free of addiction.
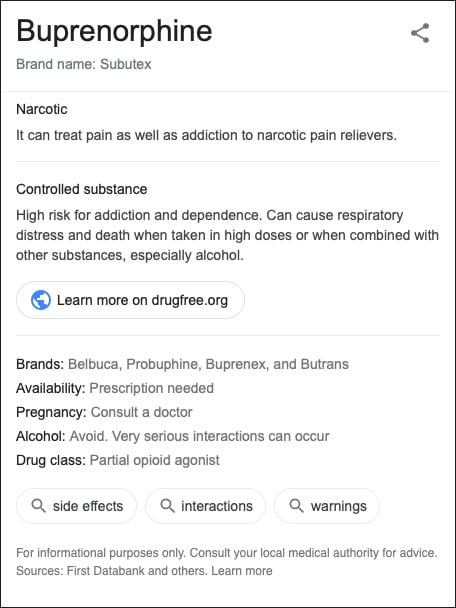
Buprenorphine hydrochloride is one such medically-assisted treatment that is meant to promote long-term recovery from opioid addiction. The generic drug is marketed under the brand names Subutex and Suboxone.
So, what is Buprenorphine? What is the difference between Suboxone and Subutex? And how can these MATs help with recovery from opioid addiction?
Buprenorphine – A Safer Alternative Against Opioid Dependence
Prior to 2000, Methadone was the primary treatment for opioid withdrawal. The drug was administered in a highly structured clinic and prescribed under controlled conditions As a Schedule II Controlled Substance, Methadone had a high potential for abuse and risk of dependence—similar to narcotics such as morphine and fentanyl.
But in 2002, the Food and Drug Administration (FDA) approved the clinical use of an equally effective but safer drug, Buprenorphine hydrochloride. Unlike Methadone, Buprenorphine is classified as a Schedule III substance—meaning its risk of physical dependence due to abuse is moderate to low.
Buprenorphine is more accessible and can be prescribed by qualified physicians and mid-level practitioners in a health department, community hospital, correctional facility, or physician office.
What is Buprenorphine?
Buprenorphine hydrochloride is a partial opiate agonist. An opiate agonist is a class of drugs that bind to opioid receptors in a person’s brain without inducing the high associated with opioid use. Full opioid agonists such as Methadone or Heroin produce maximal effects such as respiratory depression and euphoria. In other words, buprenorphine is a drug used in medically-assisted treatment to replicate the actions of highly-addictive opioid drugs—but to a lower degree.
The drug has several benefits for people battling opioid dependence, including:
- Reduce or block cravings for abused opioids such as heroin.
- Suppress opioid withdrawal symptoms.
- Increase the chance of recovery—while reducing the risk of relapse.
- Keep other opioids from attaching to receptors in the brain.
- Safely reduce dependence on other opioids.
- In the case of overdose, Buprenorphine reduces the severity of the symptoms.
Please note that Buprenorphine therapy is only one part of the rehabilitation process. It’s often prescribed as part of a comprehensive opioid rehabilitation plan—including behavioral therapies such as counseling.
How does Buprenorphine Work Against Opioid Dependence?
In a simplified explanation, Buprenorphine hydrochloride works by fooling the addicted brain into thinking that it’s receiving a dose of the abused opioid. But to understand the exact mechanism, it’s important to first understand how opioid dependence develops.
The brain of a person who doesn’t abuse opioids has a set number of opioid receptors in the brain. When heroin, fentanyl, or any other full opioid agonist is consumed, it binds to these opioid receptors—creating the high associated with the drugs.
With prolonged use, the person develops tolerance—caused by an increase in the number of opioid receptors in the brain. This creates an urge to seek more drugs or higher doses to achieve the desired level of high – i.e. it takes more drugs to fully attach to the increased number of receptors.
If the receptors are not activated due to abruptly stopping or reducing the opioid intake, withdrawal symptoms follow. The severity or intensity of the withdrawal symptoms depends on unique circumstances surrounding the drug use.
Here’s where Buprenorphine comes in: by acting as a ‘sticky agent’, the partial opioid agonist binds to the increased number of opioid receptors in the brain. This takes up the position of the abused opioids—kicking them out.
Assuming you take both Buprenorphine and Heroin at the same time, Buprenorphine pushes the Heroin away from the receptors and fills them instead. Therefore, it reduces cravings and prevents (or reduces) withdrawal symptoms without producing euphoric effects.
Is Buprenorphine Safe?
- Side Effects: As an opioid, Buprenorphine may lead to side effects such as fever, irritability, cravings, muscle aches, nausea, vomiting, and sleeping problems.
- Risk of Misuse: Although Buprenorphine hydrochloride has a significantly lower risk of dependence, it can still be abused—especially by people who haven’t been diagnosed with opioid dependence. For this reason, the drug must be prescribed or monitored by a medical professional.
- Interactions: According to the Substance Abuse and Mental Health Services Administration (SAMHSA), Buprenorphine should not be taken with other medication, alcohol, illegal drugs, or sedatives. People with existing health conditions are also advised to consult their doctors before taking Buprenorphine.
- Pregnant and Breastfeeding Women: The Federal Guidelines for Opioid Treatment Programs by SAMHSA suggests that Buprenorphine may be used for the medically-assisted treatment of pregnant or breastfeeding women with opioid dependency—but under strict supervision.
What is Subutex?
Buprenorphine is marketed under two brand names – Suboxone and Subutex. The latter is available as a tablet that is taken sublingually (i.e., dissolves under the tongue). It’s prescribed by a qualified doctor in either 8 mg or 2 mg single daily dose—with the intention to gradually reduce the dosage over time.
And since Buprenorphine is the main active agent in Subutex, it works in the same way by binding to opioid receptors without inducing the a high or CNS suppression.
Similar to Buprenorphine, Subutex may interact with other drugs such as phenytoin, theophylline, metronidazole, warfarin, isoniazid, tricyclic antidepressants, benzodiazepines, and monoamine oxidase inhibitors (MAOIs), among others. In other words, always consult your doctor if you’re using other drugs.
Please note that when snorted or injected intravenously in large doses, Subutex can cause severe symptoms such as unconsciousness, confusion, dizziness, or suppression of breathing and possibly Tardive Dyskinesia.
Common Side Effects of Subutex
Along with its beneficial effects, Subutex may cause some undesirable side effects. Some are rare, while are more common—including:
- Runny nose
- Back pain
- Constipation
- Chills
- Stuffy nose
- Trouble sleeping
- Difficult urination
- Hoarseness
- Cough
- Sneezing
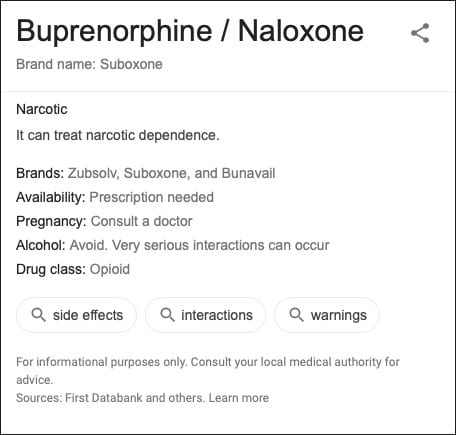
What is Suboxone?
Suboxone is another brand name for Buprenorphine hydrochloride, but with one major difference from Subutex – i.e., it’s combined with Naloxone.
Naloxone is an FDA-approved full opioid antagonist. This means that instead of exciting opioid receptors—as is the case with opioid agonists such as Buprenorphine—Naloxone shuts them down. It temporarily reverses the effects of other opioids. According to a study published in the Journal of Addiction, Suboxone is an effective medically-assisted treatment.
Suboxone is administered sublingually in either tablet form or as an oral film to be placed under the tongue. The film can also be taken buccally—whereby it’s placed between the cheek and gums to dissolve. When consumed sublingually (as it’s meant to be administered) it’s relatively inactive and you don’t feel the effects. But when snorted, dissolved, or injected, Naloxone blocks the opioid receptors—countering the effects of the opioids.
Buprenorphine was combined with Naloxone to create Suboxone with the intention to discourage users from abusing the Buprenorphine. But despite this, some users still find ways to abuse the drug. Since Buprenorphine has a longer half-life than Naloxone, it’s possible to snort or inject Suboxone in high enough doses and wait for the Naloxone to wear off.
Drugs that have been shown to interact with Suboxone include Acetaminophen, HIV-treatment drugs, Niacin, Cholesterol-lowering medications, Oral contraceptives, Fluoxetine, and Verapamil
Possible Side Effects of Suboxone
Some common side effects of Suboxone include:
- Headache
- Dizziness, drowsiness
- Blurred vision
- Numbness or redness inside your mouth
- Trouble concentrating
- Sleep problems
- Nausea or vomiting
- Withdrawal symptoms
- Tongue pain
- Constipation
- Increased sweating
Suboxone Vs Subutex – Which One is Better?
Keep in mind that the decision between Suboxone or Subutex should be left to a qualified and licensed medical professional. But nonetheless, this is a relatively common question among users—especially since they both contain the same active compound and serve the same function.
The most notable way to differentiate between Suboxone and Subutex is in the role of Naloxone. For example, if you have a history of Buprenorphine addiction or you’re at high risk of relapse, Suboxone may be the better choice. Since Naloxone blocks and counteracts the effects of abused opioids, users who relapse may not experience the high that they’re looking for in the drugs. Suboxone is also less likely to be abused—again, owing to the addition of Naloxone.
But if you’re strapped for cash and you want an effective medically-assisted treatment, you may be better placed to use Subutex. By virtue of containing Buprenorphine as the only active ingredient, Subutex is relatively cheaper.
It’s important to note that although Suboxone and Subutex contain the same active compound, switching from one drug to the other is not a straightforward process. Doing so without careful planning and medical advice may lead to adverse effects.
In a 2008 study appearing in Substance Abuse Treatment, Prevention, and Policy, 26.6% of patients who switched from Subutex to Suboxone at the same dose reported adverse effects. The switch was made as an attempt to curb the rising cases of Subutex abuse. The researchers concluded that “We recommend that a transfer from Subutex to Suboxone should be carefully discussed and planned in advance with the patients and after the transfer adverse events should be regularly monitored.”
Research on the Effectiveness of Buprenorphine
- In a study published in the Journal of Drug and Alcohol Dependence, patients with heroin dependence reported a greater reduction in heroin use and adverse side effects after 3 months of using Suboxone.
- According to the findings from a Swedish study appearing in The Lancet, 75% of patients who used buprenorphine remained in treatment compared to 0% in a placebo group. In other words, placebo treatment had a 100% failure rate—compared to buprenorphine treatment that only had a 25% failure rate.
- A study in the Journal of Addiction and Research Therapy concluded that “Buprenorphine (BUP) is an effective treatment option for achieving abstinence from opioids, and with emerging treatment guidelines, may be easier to access than other forms of treatment.”
- Evidence shows that Buprenorphine is effective in maintaining patient retention at all doses—but it’s most effective at doses of around 16 mg daily.
Who Needs Opioid Use Disorder Treatment?
A person with two or more of the following symptoms within a 12-month period may need to seek opioid detox and addiction treatment services.
- An urge or craving to use opioids.
- Inability to control or cut down opioid use.
- Spending a significant amount of time and resources obtaining, using, or recovering from the effects of opioid use.
- Problems and conflicts at home, school, or work.
- Interpersonal and social problems due to opioid use.
- Building tolerance to the abused opioid.
- Ongoing psychological and physical problems caused by opioids—but you still continue using the substances.
- Withdrawal symptoms
Addiction Treatment with Subutex and Suboxone
Addiction to opioids has far-reaching consequences at an individual and national level. Medically-assisted treatments such as Suboxone and Subutex help people overcome opioid use disorder—and consequently curb the opioid epidemic ravaging the United States.
Addiction treatment starts with an accurate diagnosis of opioid dependence. The candidate should also be willing and ready to follow any safety precautions necessary for his or her recovery. It’s also important to assess the health condition of the person with opioid dependency.
MAT using Suboxone or Subutex typically happens in 3 phases:
- In the induction phase, Buprenorphine is administered for the first time after the patient has abstained for at least 12 hours. At this stage, the person with an opioid dependency is likely in the early stages of withdrawal.
- After the patient shows a significant reduction in side effects, cravings, and misuse of the opioid, they advance to the stabilization phase. Depending on the progress, the dosage may need to be adjusted.
- The final phase of medically-assisted treatment opioid abuse disorder is known as the maintenance phase. The patient is recovering and making steady progress. The aim is to prevent relapse and promote the long-term recovery of the person with an opioid dependency.
Suboxone and Subutex should not be used alone for the treatment of addiction. They are most effective when used as part of a comprehensive treatment program—including different evidence-based therapies, counseling programs, holistic therapies, or self-help programs.
Related: Suboxone Withdrawal
Help is Available at Revive Detox!
Medically-assisted treatment provides a strong foundation for safe recovery and healthier, happier life. If you or your loved one is ready to take the next steps to break free from the chain of opioid addiction, Revive Detox is here to help. Seeking help is a momentous decision toward recovery.
We employ the best medical practices and proper attention to ensure your treatment is as comfortable as possible. Our programs are patient-centered and tailored to your unique needs—hence improving the outcome. For more on how Revive Detox can help you overcome opioid addiction, call us at (844) 467-3848.