An atrophic pancreas refers to inflammation and progressive damage to the pancreas resulting in deteriorating pancreatic function.
Alcohol consumption is one of the leading causes of pancreatitis that can eventually lead to an atrophied, non-functioning organ.
How Alcohol Causes Pancreatitis and Pancreatic Atrophy
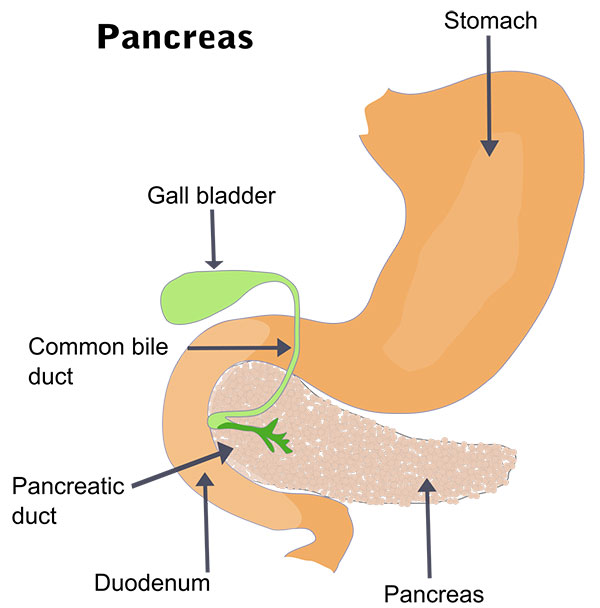
The pancreas produces enzymes and hormones crucial for digestion.
Long-term heavy alcohol intake frequently causes repeated attacks of acute inflammation in the pancreas, resulting in permanent injury over time.
Alcohol and its byproducts directly damage pancreatic cells and ducts. This impairs secretion of digestive enzymes, leading to atrophy.
Specifically, alcohol boosts fat levels in pancreatic juices.
The alkalinized fatty acids combine with calcium in the pancreatic juices to form soap-like precipitates that clog ducts and cause pancreatic autodigestion and cell destruction.
With repeated acute flareups, progressive irreversible atrophy of the pancreas develops along with a severe deficiency of the enzymes and hormones it produces.
Let’s examine this process in further detail.
Stages of Alcoholic Pancreatitis Leading to Atrophy
Acute Alcoholic Pancreatitis
The early and reversible stage of alcoholic injury to the pancreas is known as acute pancreatitis.
It may occur suddenly, caused by excessive alcohol intake in a short period. Symptoms are usually severe and require hospitalization.
With alcohol abstinence and treatment, acute flareups can resolve without permanent damage.
However, repeated episodes lead to increasing destruction and dysfunction of the pancreas.
Chronic Alcoholic Pancreatitis
In the chronic phase, prolonged alcohol misuse causes fibrosis and calcification of pancreatic tissue as well as destruction of exocrine and endocrine cells.
Pain becomes persistent rather than intermittent attacks. Maldigestion leads to vitamin deficiencies and malnutrition.
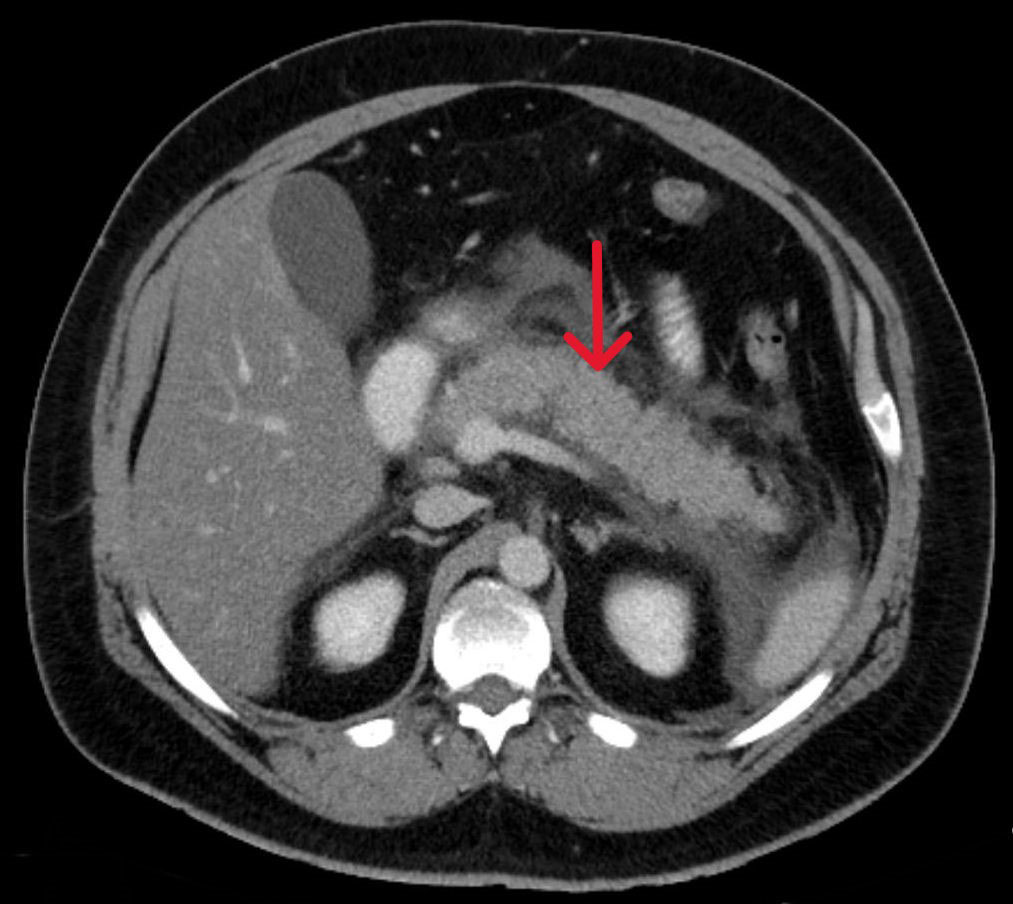
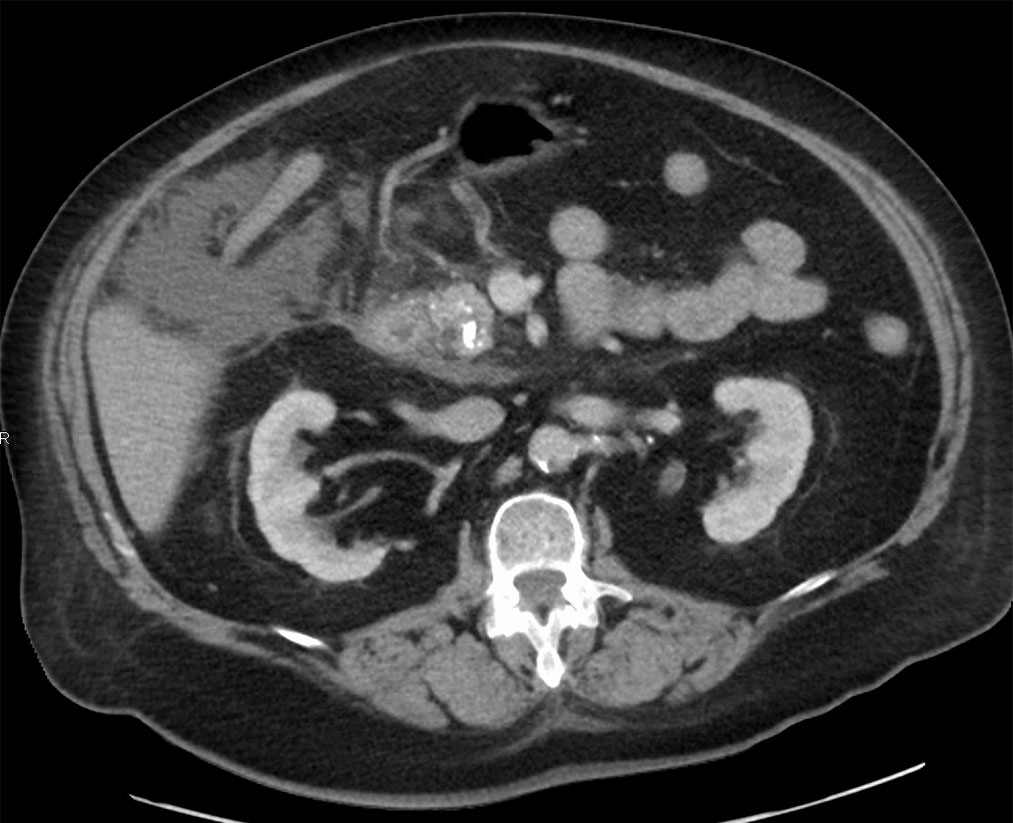
Necrosis and calcification visible on CT scans indicate advanced chronic pancreatitis.
The gland becomes rock-hard with extensive scarring and calcified deposits.
Patients develop issues like diabetes and steatorrhea at this stage.
Pancreatic Atrophy
In the final stage, the pancreatic structure is extremely distorted with widespread cell loss and fibrosis leading to a shrunken, non-functional gland unable to produce enzymes or hormones in sufficient amounts.
Ultimately, end-stage chronic alcoholic pancreatitis results in severe exocrine and endocrine insufficiency – termed atrophic pancreatitis.
The damaged pancreas cannot synthesize or secrete digestive juices (exocrine function) or regulate glucose via insulin (endocrine function).
Diagnosing Atrophic Pancreatitis
Since patients are often asymptomatic in early stages, clinicians rely on imaging and lab tests for diagnosis. These include:
- Serum trypsinogen and fecal elastase tests to assess exocrine function
- Fasting blood glucose and HbA1c for endocrine function
- MRI and CT scans to visualize pancreatic atrophy, calcification, cysts
- Endoscopic ultrasound (EUS) to check structural damage
- ERCP (endoscopic retrograde cholangiopancreatography) using contrast dye to see ductal structural changes
Complications of Chronic Atrophic Pancreatitis
Exocrine Insufficiency
With extensive damage and fibrosis of pancreatic tissue, patients develop malabsorption and deficiency of fat-soluble vitamins A, D, E and K.
Steatorrhea, weight loss, and malnutrition result due to lack of pancreatic digestive enzymes (lipase, amylase, trypsin).
Endocrine Insufficiency
Loss of insulin-producing beta cells over time leads to diabetes in over 80% of patients with chronic pancreatitis.
This is challenging to control owing to poor glucose tolerance and appetite loss.
Increased Risk of Pancreatic Cancer
Chronic inflammation significantly raises the risk of pancreatic adenocarcinoma.
Patients require regular screening via imaging and tumor marker tests.
Associated Conditions
Celiac disease, Crohn’s disease, lipomatosis of the pancreas and ulcerative colitis tend to co-occur with chronic pancreatitis.
As liver and pancreas disease frequently overlap, many patients also suffer from cirrhosis, hepatitis, or fatty liver.
Chronic pancreatitis also aggravates liver disease and vice-versa.
Treatment Approaches for Atrophic Pancreatitis
The treatment strategy focuses on slowing down progression, managing symptoms, replacing lost function, and monitoring complications via:
- Abstinence from alcohol to stabilize disease
- Pain control via analgesics
- Pancreatic enzyme supplements
- Insulin or other drugs for diabetes
- Surgery if bile ducts are blocked or large cysts develop
- Nutritional support to prevent weight loss
- Screening for and treating malignancies
- Treatment for associated conditions like cirrhosis
Preventing Pancreatic Atrophy
Since alcohol is the most common causative factor for chronic pancreatitis and subsequent atrophy, abstinence is critical, especially in high-risk individuals.
Even after disease onset, stopping alcohol intake can substantially slow down progression. Beyond alcohol avoidance, other preventive strategies include:
- Maintaining normal weight
- Avoiding dietary fat and processed red meat
- Taking antioxidants and folate
- Drinking more water to flush out ducts
Early intervention is also key.
Seeking prompt treatment for acute pancreatitis flareups via fluids, bowel rest, and pain management helps minimize permanent harm and prevent infiltration and progression to chronic pancreatitis and, ultimately, pancreatic atrophy.
Coping with an Atrophic Pancreas
Living with lost pancreatic function can be extremely challenging. Making appropriate lifestyle changes and adhering to treatment under medical supervision can help patients cope better.
Tips include:
- Joining a patient support group
- Discussing job accommodations if needed
- Adopting low-fat, high-protein, anti-inflammatory diets
- Taking extra care to avoid infections
- Monitoring blood sugar and taking insulin properly
- Using vitamin supplements if deficient
- Avoiding behaviors that exacerbate disease
- Seeing a therapist or counselor for emotional health
With the right treatment plan and dedicated self-care, patients can adapt to living with exocrine and endocrine insufficiency resulting from advanced chronic pancreatitis leading to atrophy.
The outlook depends greatly on alcohol abstinence and early intervention.
FAQs
Can Atrophic Pancreas be Reversed?
Reversing atrophic pancreas is a complex issue, as the damage to the pancreas is often irreversible.
However, in some cases, addressing the underlying cause of the atrophy can help slow down or stop further damage to the pancreas.
For example, managing conditions like chronic pancreatitis or reducing alcohol consumption can help preserve pancreatic function.
Additionally, certain treatments, such as enzyme replacement therapy, may help improve digestion and overall pancreatic function.
It is important to consult with a healthcare professional to discuss treatment options and to develop an individualized plan for managing atrophic pancreas.
While complete reversal of atrophic pancreas may not always be possible, taking steps to address the underlying causes and manage symptoms can greatly improve quality of life for those affected by this condition.
What is the Life Expectancy of Someone with Chronic Pancreatitis?
The life expectancy of someone with chronic pancreatitis can vary depending on the severity of the condition and the individual’s overall health.
In general, studies have shown that the life expectancy of individuals with chronic pancreatitis is reduced compared to the general population.
However, with proper management of symptoms, treatment of complications, and lifestyle changes such as abstaining from alcohol and following a healthy diet, it is possible to improve the quality of life and prolong the lifespan of someone with chronic pancreatitis.
It’s important for individuals with chronic pancreatitis to work closely with their healthcare providers to develop a comprehensive treatment plan and to monitor and address any potential complications to optimize their long-term prognosis.